AI Infusion™ works by breaking complex operations into discrete workflow components and identifying the dominant activity types within each. This allows us to pinpoint exactly where labor, cost, and operational risk are concentrated inside a benefits administration organization. The workflows below highlight those concentration points.
On the next page, we go one level deeper into each activity type and outline the specific AI Infusion™ patterns that streamline execution, reduce cost, and improve accuracy — while preserving human oversight where it matters.
For a hypothetical company that has 100 FTEs in the back office, here are the projected improvements in the top 10 workflows:
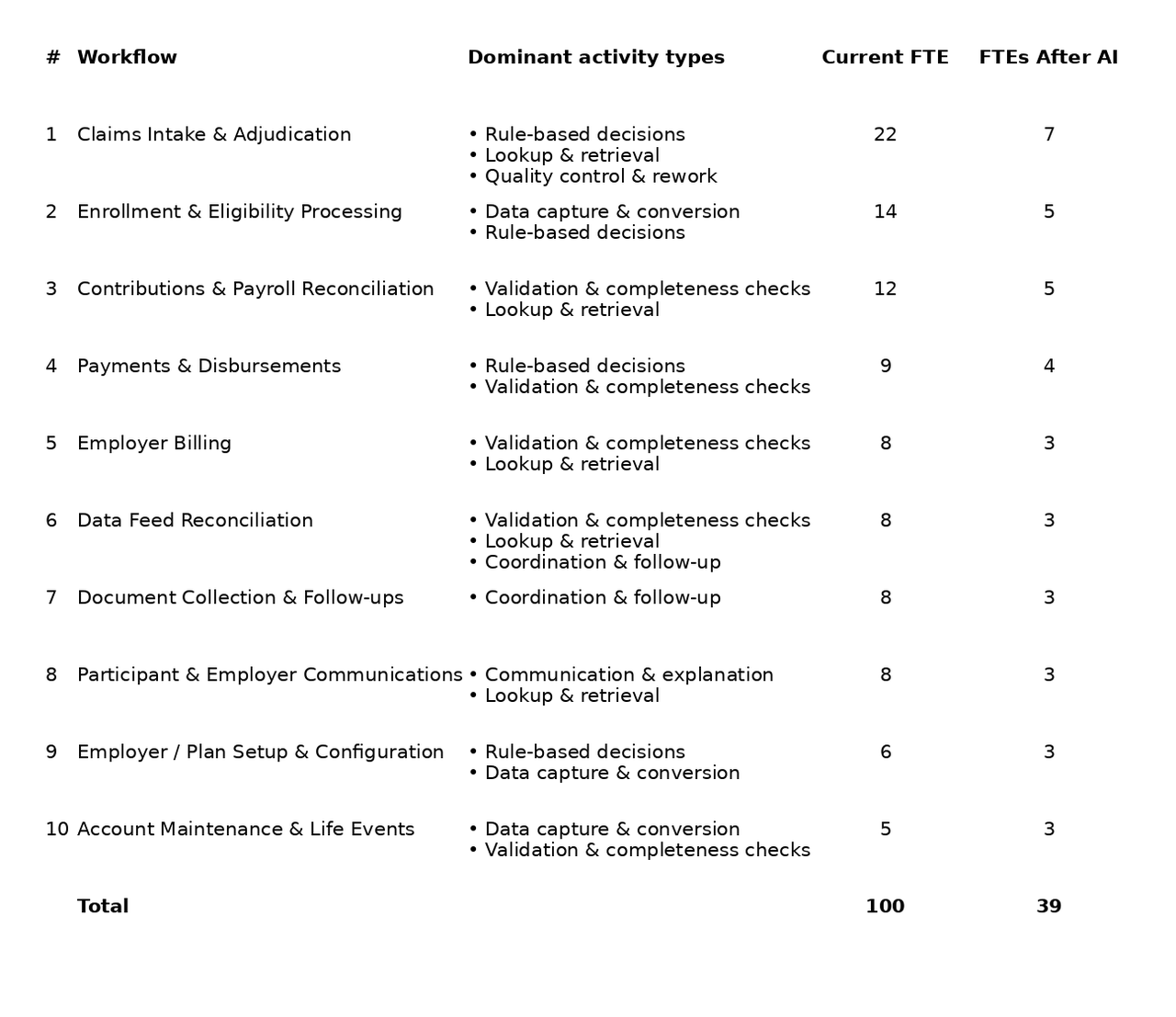
These estimates are based on our experience across multiple real-world engagements. Actual results vary by environment, scale, and adoption model.
Let’s take a deeper look at each workflow.
What it is
The end-to-end evaluation of participant reimbursement requests. This includes intake of claim data, verification of eligibility and balances, application of plan rules and regulatory requirements, determination of approval or denial, calculation of payable amounts, and documentation of the decision. It is typically the highest-volume and most resource-intensive workflow in benefits administration.
Primary activity types
What it is
The process of establishing and maintaining participant eligibility based on employment data, employer configurations, effective dates, and governing plan rules. This workflow ensures that individuals are correctly enrolled in the appropriate benefit plan and that downstream transactions align with coverage status.
Primary activity types
What it is
The reconciliation of payroll deductions, employer contributions, and participant account balances across administrative and financial systems. This workflow ensures that funding levels match plan elections, payroll feeds, and system records, and that discrepancies are identified and resolved promptly.
Primary activity types
What it is
The operational execution of participant reimbursements and employer-related fund transfers. This includes validation of payment eligibility, calculation of payable amounts, issuance of payments, and management of corrections, voids, or reversals. Accuracy and timeliness are critical, as this workflow directly impacts participant experience and financial compliance.
Primary activity types
What it is
The generation, validation, and reconciliation of invoices issued to employer clients for administrative fees, funding requirements, and service-related charges. This workflow ensures that billing reflects contractual terms, aligns with actual plan activity, and withstands audit or dispute scrutiny.
Primary activity types
What it is
The operational oversight of inbound and outbound eligibility and payroll data feeds exchanged between employers, payroll providers, carriers, and administrative platforms. While file transmission is automated, this workflow manages validation failures, reject reports, record mismatches, and reconciliation discrepancies to maintain cross-system data integrity.
Primary activity types
What it is
The structured pursuit of required documentation needed to advance claims, eligibility updates, or compliance requirements. This includes tracking pending items, issuing reminders, monitoring deadlines, and escalating overdue responses to prevent case stagnation.
Primary activity types
What it is
The preparation and delivery of structured explanations related to claims outcomes, documentation requirements, eligibility determinations, account activity, and next steps. Communications must align with plan rules, regulatory standards, and service expectations while maintaining clarity and consistency.
Primary activity types
What it is
The translation of contractual benefit designs and employer-specific policies into executable system configurations. This includes defining eligibility logic, contribution limits, claims rules, plan parameters, and reporting structures so that operational systems accurately reflect agreed plan designs.
Primary activity types
What it is
The ongoing maintenance of participant records due to employment changes, qualifying life events, demographic updates, corrections, or administrative adjustments. This workflow ensures that account data remains accurate and aligned with coverage status throughout the participant lifecycle.
Primary activity types